Tap Into Your Water: Transform Care and ROI

Water is not just a utility in healthcare. It is a critical part of patient safety, operational performance, and financial stability. Yet, for many organizations, water risk remains hidden until it leads to a costly disruption or outbreak. For healthcare leaders, managing water is a strategic decision that protects patients, strengthens compliance, and safeguards margins. With a proactive, multi-barrier water management approach, hospitals can turn water into an asset that drives safety, resilience, and return on investment. Patient safety and experience Clean water drives safer care and better outcomes The challenge Waterborne pathogens like Legionella, Pseudomonas, and nontuberculous mycobacteria (NTM) are an often-overlooked source of healthcare-associated infections (HAIs). According to research, water can be a source for more than 20% of HAIs. These infections compromise patient safety, erode trust, and negatively affect patient experience scores such as HCAHPS. For healthcare, every infection linked to water systems represents both a human risk and a reputational liability. The impact Waterborne HAIs increase length of stay, reduce capacity, and can cause value-based reimbursement penalties. They can also create negative headlines that damage community trust and competitive standing. Over time, financial and reputational costs compound, diverting resources from growth, innovation, and patient care. The solution LiquiTech reduces infection risks at the source with a multi-barrier approach that removes sediment, eliminates pathogens, prevents regrowth, and protects plumbing infrastructure. This extends the life of water-bearing equipment, reduces energy inefficiencies, and creates a safer environment for patients and staff. Proactive protection helps preserve infrastructure, deliver better outcomes, safeguard reputation, and reduce operating costs. Financial margin protection Safety delivers measurable ROI The challenge Shrinking margins, labor pressures, and rising operational costs leave little room for unplanned crises. A single outbreak or infrastructure failure can drain millions in unbudgeted expenses and force capital reallocation away from strategic priorities. The impact Emergency remediation, litigation, reputational damage, and lost revenue from closed units or diverted patients all strain budgets. Premature infrastructure replacement or plumbing repairs further erode financial stability. These avoidable costs undermine investments in technology, workforce development, and patient care innovation. The solution LiquiTech protects financial margins by preventing outbreaks and extending the life of plumbing systems and equipment. Our solutions reduce emergency remediation, lower energy inefficiencies, and cut premature replacement costs. By reducing the total cost of risk, we free up capital to reinvest in advancing patient care, enhancing staff resources, and strengthening long-term financial performance. Regulatory compliance Compliance you can prove The challenge Organizations such as the Joint Commission, CMS, DNV, and ASHRAE require defensible water management programs with governance, monitoring, and testing. Without a comprehensive, verifiable plan, healthcare organizations face serious compliance gaps and increased risk during survey. The impact Survey failures can result in penalties, fines, or even loss of accreditation. Beyond the immediate financial consequences, non-compliance undermines leadership credibility and disrupts reimbursements. Gaps in documentation create unnecessary stress for staff and leadership alike. The solution LiquiTech designs and manages tailored water management programs aligned with every requirement. With monitoring, testing, and defensible reporting, you are always survey-ready, not just during inspections. This transforms compliance from a liability into a source of leadership confidence, reducing risk and freeing staff to focus on patient care. Enterprise risk and resilience Resilient hospitals start with resilient water The challenge Hospital operations rely on water for every function, from sterile processing to patient care. Yet risks often remain invisible until a crisis occurs. Outbreaks, pipe failures, or contamination events can rapidly shut down units and disrupt continuity of care, destabilize operations, and tarnish brand reputation for an entire organization. The impact Service interruptions force diversions, cancel procedures, and undermine trust with patients, staff, and communities. Each incident risks regulatory investigations, lawsuits, and reputational harm. When water systems fail, organizational resilience and the ability to deliver reliable care are compromised. The solution LiquiTech builds resilience into water systems with smart monitoring, rapid-response playbooks, and preventive strategies. By detecting risks early and ensuring infrastructure reliability, disruptions are minimized, equipment life is extended, and energy inefficiencies are reduced. This proactive approach ensures uninterrupted care, reputation, and operational resilience even when external pressures mount. Sustainability and ESG Safer for patients, smarter for the planet The challenge Hospitals face rising expectations to meet ESG goals while protecting patients and infrastructure. Traditional chemical treatments introduce harmful byproducts, accelerate corrosion, and increase energy demand and long-term costs, all while putting sustainability at odds with safety. The impact Chemical approaches are outdated, drive premature system failures, raise energy consumption, and create environmental hazards. They also raise concerns from patients, staff, and communities who expect environmentally responsible care. Failing to adopt sustainable practices risks reputational harm and higher operational costs. The solution LiquiTech’s multi-barrier approach eliminates pathogens without harmful byproducts. By reducing corrosion, extending equipment life, and lowering energy use, we protect both people and infrastructure. Our solutions help hospitals meet ESG goals while delivering safer, smarter, and more sustainable care. Tap into the hidden potential of water Water touches every part of your healthcare system, from patient safety and compliance to finances and sustainability. By managing it strategically, you can transform an overlooked operational risk into a driver of measurable improvement and resilience. LiquiTech’s multi-barrier solutions empower healthcare leaders to strengthen water safety, reduce costs, and protect their facilities for the future. It is time to take a proactive step Connect with our team today to learn how smarter water management can help your organization achieve safer care, stronger performance, and better ROI.
The Broader Impact of Effective Water Management

Water safety is often focused only on Legionella control, but an effective program can provide a much wider range of benefits. Water quality influences not only occupant health but also the performance of infrastructure, long-term sustainability goals, and financial outcomes. When facilities rely on outdated or incomplete water management strategies, they leave themselves vulnerable to risks that go well beyond Legionella. A smarter approach, grounded in a multi-barrier water management strategy, offers a way to protect people, extend equipment life, reduce operational costs, and support sustainability. Why traditional water treatment methods fall short Many facilities continue to lean on conventional practices such as flushing, temperature monitoring, and municipal disinfectant residuals. While these measures are widely used, they rarely address the real drivers of waterborne pathogen risk. Biofilm and sediment shield bacteria from disinfectants, temperature control is ineffective, cold water risks are overlooked, and flushing programs often require significant time and energy without producing lasting results. The cycle of monitoring and corrective actions that results from these methods is not just inefficient; it can mask bigger problems, such as hidden sediment accumulation or corrosion that undermines water quality throughout a building. The overlooked role of sediment Sediment is an underestimated challenge in building water systems. Sediment is naturally present in source water and often introduced through water main breaks, construction activity, or corrosion within pipes. Once inside, it quietly disrupts both water quality and infrastructure: Sediment-induced damage Broader impacts on facilities Poor water management is not just a safety concern; it affects every part of a facility’s operation. This interconnected risk landscape is why leading facilities are rethinking their approach with multi-barrier solutions that go beyond Legionella and compliance. Smarter water management A multi-barrier approach layers proven technologies with expert service to create a comprehensive, defensible water management strategy. Together, these measures protect both people and infrastructure: These technologies are integrated into a program supported by data analytics and remote monitoring, ensuring that facility teams can act proactively instead of reactively. Real-world results The benefits of this approach are measurable. In one academic medical center, implementing a multi-barrier solution allowed hot water heaters to be lowered from 160°F to 125°F while still achieving non-detect Legionella results, cutting energy use by 50%. Another facility reduced sediment loads by nearly 98%, preventing costly pump failures and improving system reliability. Even more importantly, infection risk was significantly reduced. One facility saw complete elimination of Pseudomonas, Acinetobacter, and Stenotrophomonas detections, improving patient safety and reducing the burden of HAIs. Rethink water safety for the future Water is more than a utility; it’s a clinical, operational, and financial risk factor. By addressing underlying issues like sediment and biofilm with smarter, layered protection, facilities can safeguard their people, extend equipment life, and achieve long-term results. If your current water management strategy feels like a cycle of short-term fixes, it may be time to take a smarter approach. Connect with a LiquiTech water safety expert today to explore how a multi-barrier strategy can transform your facility’s water quality and performance.
Multi-Barrier Approach: Setting a New Standard for Water Safety

Healthcare facilities today face increasing water safety risks. Aging infrastructure, frequent water main breaks, and elevated sediment levels are straining plumbing systems and creating ideal conditions for waterborne pathogens to thrive. Municipal treatment processes, while essential, often don’t address these downstream challenges once water enters a facility. The result is a growing concern for occupant safety, equipment reliability, and compliance. One healthcare facility confronted these realities head-on after dealing with Legionella positivity in its cold-water system, as well as recurring detection of Pseudomonas, Acinetobacter, and Stenotrophomonas. Beyond microbial risks, high sediment loads from the municipal water supply were causing significant damage to plumbing infrastructure, increasing maintenance costs, and accelerating corrosion. Traditional remediation approaches were unable to deliver sustainable results. The Challenge The facility needed a comprehensive strategy that could both eliminate pathogens and reduce the environmental conditions that allowed them to flourish. The solution: A multi-barrier approach To address these challenges, LiquiTech implemented a multi-barrier water treatment solution designed to deliver layered protection: Together, these technologies worked in synergy to address the root causes of water quality problems and provide sustained protection. The results By addressing microbial challenges, sediment-related damage, and infrastructure reliability together, the facility established a new standard of care for water safety. The solution not only safeguarded patients and staff but also delivered measurable operational and financial benefits. Connect with an expert Fill out the form below to connect with a LiquiTech expert to explore how a multi-barrier water treatment approach can help protect your facility’s water, systems, and ROI.
AAMI ST108: Ensuring Water Quality in Medical Device Processing

The Association for the Advancement of Medical Instrumentation (AAMI) introduced Standard ST108 in 2023 to replace the previous AAMI TIR34:2014/(R)2021 standard. AAMI ST108 includes guidelines on: Categories of water quality: Defines water quality requirements for each stage of sterile processing. Water quality monitoring: Sets criteria for assessing water quality, including turbidity, pH, microbial levels, conductivity, and other factors. Water treatment: Establishes protocols for maintenance, monitoring, and quality improvement in water treatment systems. AAMI ST108 is considered a best practice for patient safety and is likely to become a requirement of other standards, like The Joint Commission Water Management Standard EC.02.05.02. Categories of water quality AAMI ST108 standardizes water quality for medical device processing to prevent adverse outcomes associated with substandard water. It defines three primary water quality levels—utility, critical, and steam—each tailored to different stages of device sterilization and disinfection. Utility water or tap water is generally minimally processed and used for tasks like flushing and washing. Critical water requires higher purity levels for tasks like high-level disinfection and final rinsing. Steam is used in sterilization and must meet specific standards to ensure safety and efficacy. The standard includes extensive testing protocols to ensure water quality across these categories. Key testing criteria include turbidity, pH, microbial levels, conductivity, and various chemical parameters. Water quality monitoring To comply with ST108, facilities must routinely test utility, steam, and critical water to ensure consistent quality. Water testing should cover microbial and chemical parameters as well as general water quality metrics like turbidity, pH, and total organic carbon. Routine testing frequency is determined based on initial validations and risk assessments, with periodic testing following interruptions, repairs, water advisories, or in response to adverse outcomes (e.g., staining, discoloration, or deposits on medical equipment). Facilities should create sample locations representative of water contact points and monitor this over time to ensure ongoing compliance with ST108 standards. All water quality parameters, monitoring and verification protocols, and control measures should be incorporated into the facility’s existing water management plan. Water treatment In the ST108 sterilization process, water treatment is divided into three main stages: pretreatment, primary treatment, and storage/distribution/final treatment. Each stage is essential in preparing high-purity, sterile water for medical and sterilization equipment. Here’s a breakdown of how these stages are structured. Stage 1: Pretreatment The pretreatment stage prepares water for further purification. This step ensures that downstream equipment operates efficiently by removing larger particles, sediments, chlorine, and hardness, which could cause damage or interfere with subsequent treatments. Sediment filtration: Filters particles and sediment from the utility water that could harbor bacteria or clog and damage equipment. Carbon filtration: Dechlorinates water by removing chlorine and organic compounds. Water softening: Reduces hardness (calcium and magnesium) to prevent scaling and extend equipment life. Stage 2: Primary treatment The primary treatment stage refines water quality to meet strict purity and safety standards, making it suitable for medical sterilization applications. The goal of this stage is to achieve high levels of purity by removing dissolved ions, organic contaminants, and microorganisms. Reverse osmosis (RO): Uses a semipermeable membrane to filter out ions, organic matter, and some microorganisms, creating purified water. Deionization (DI): Uses ion-exchange resins to further purify the water by removing any remaining dissolved salts and ions. Stage 3: Storage, distribution, and final treatment This stage maintains water quality during storage and distribution and ensures the highest purity right before use. The purpose of this stage is to prevent microbial contamination and ensure that water remains sterile at the point of use. UV disinfection: Provides final microbial inactivation by using UV light to disrupt bacterial DNA. Point-of-use filtration: Use of micropore or ultrafine filters at the final outlet to prevent contaminants from entering the sterilization cycle. Incorporating ST108 into your water management program To incorporate ST108 into your water management plan, start by reviewing your current water treatment processes and identifying areas that need alignment with ST108’s requirements. Involve key personnel such as facility managers, infection preventionists, clinical engineering staff, medical device processing personnel, and water safety specialists who understand both operational needs and regulatory standards. These specialists will assess your existing setup, identify gaps, and update treatment protocols to ensure compliance. Collaborate with water treatment experts to implement technologies that meet ST108 criteria at each stage of water handling, from pretreatment to storage and distribution. For example, they may recommend sediment filtration, softening, or UV disinfection systems tailored to your facility’s usage patterns and contaminant profile. Additionally, integrate regular testing and monitoring into your water management plan to ensure ongoing compliance and make adjustments to processes as needed. Partnering with LiquiTech to comply with ST108 LiquiTech simplifies ST108 compliance with targeted solutions that streamline water quality monitoring and control. Water quality testing facilitation Coordination services to streamline ST108 testing compliance. Automatic shipment of sampling bottles and coordination with third-party labs. Water management program integration Support in incorporating ST108 guidelines into your water management plan. LiquiTech™ Sediment Filtration (pretreatment) Removes particulates from utility water to meet ST108 standards, making it suitable for critical applications. Protects reverse osmosis (RO) and deionization (DI) systems by reducing fouling and scaling, which extends equipment lifespan and lowers maintenance costs. Minimizes biofilm formation to reduce microbial risks. Ready to get started? Contact LiquiTech today to see how we can help your facility comply with AAMI ST108.
CDC Report: Burkholderia multivorans Infections Linked to Hospital Ice Machines
A Centers for Disease Control and Prevention (CDC) report published on October 3, 2024, linked Burkholderia multivorans infections to ice machines in multiple healthcare facilities in the western United States. This post summarizes key findings, implications, and recommended practices for healthcare providers to ensure patient safety. Background Burkholderia multivorans, a member of the Burkholderia cepacia complex, is an opportunistic pathogen commonly found in soil and water. It poses a significant risk to immunocompromised patients, leading to severe infections. Previous outbreaks have linked this bacterium to contaminated medications and medical devices. However, a recent investigation linked the use of ice and water from ice machines in hospitals as a potential transmission route. Between 2021 and 2022, 23 cases of Burkholderia multivorans were reported at two hospitals in Southern California. Further investigations revealed an additional 23 previously unreported cases between 2020 and 2024 across various hospitals in California and Colorado. All affected facilities used the same brand of ice machines, filters, and cleaning products, suggesting a common source of contamination. Investigation findings The investigation defined cases as infections from the outbreak strain (ST659) of Burkholderia multivorans in patients without cystic fibrosis. A total of 46 cases were identified across four hospitals: Environmental sampling indicated that B. multivorans was isolated from ice machines at some of these hospitals, confirming the link between contaminated ice and clinical cases. Genomic testing revealed that the clinical and environmental isolates were genetically similar, with only minor variations. This reinforces the hypothesis that contaminated ice machines were a significant source of exposure for patients. Recommendations for healthcare facilities Given the serious nature of these findings, the report emphasizes the need for healthcare facilities to implement robust infection control measures. Key recommendations include: The association between Burkholderia multivorans infections and ice machines in healthcare settings underscores the critical need for vigilance in infection control practices. By taking proactive measures like implementing a comprehensive water management program and adopting building water treatment technologies, healthcare facilities can minimize the risk of contamination and protect vulnerable patients from serious infections.
Plumbing 201 for Infection Preventionists: The Impact of Plumbing on Healthcare

Healthcare facilities are tasked with preventing the spread of healthcare-associated infections (HAIs), and the intricacies of plumbing design and material selection play a significant role in this effort. The role of biofilm in promoting bacteria and pathogens in healthcare water systems including drains and the link between drinking water outbreaks like Legionella to biofilm in plumbing systems, and the importance of selecting the right materials for supply lines are all pivotal in curbing the risk of HAIs. The role of plumbing in infection control Understanding the interaction between plumbing materials and microbial growth is imperative for Infection Preventionists (IPs). Making informed choices during construction and renovation allows for the selection of materials that not only minimize infection risks but also ensure compliance with health and safety standards. By collaborating effectively with facility management, IPs can significantly contribute to joint infection control initiatives, ensuring that plumbing systems do not become a source of infection. Key plumbing terms to understand Infection prevention requires a firm grasp of key plumbing concepts that impact patient safety. Understanding terms such as leaching, corrosion, and biofilms enriches an IP’s toolkit, allowing for better mitigation of risks associated with waterborne infections. Leaching The process by which materials, such as metals or chemicals, dissolve or are washed out from the pipe material into the water due to contact with the water over time. In healthcare settings, leaching can introduce potentially harmful substances into the water supply, affecting water quality and patient safety. Corrosion The gradual destruction or deterioration of materials (metals, alloys, plastics, etc.) caused by chemical reactions with their environment. In pipes, corrosion can lead to reduced water flow, leaks, and the release of metals into the water, which can serve as nutrients for microbial growth, including biofilms. Biofilm A complex aggregation of microorganisms, including bacteria, fungi, and protozoa, that adhere to each other and surfaces, encased in a protective and adhesive matrix. Biofilms in plumbing systems can harbor pathogens, making them resistant to disinfection and posing a significant risk for HAIs. Types of lines: Supply, return, drain, waste Plumbing systems consist of multiple types of lines, each with a distinct function. Here, we explore supply lines, return lines, drain lines, and waste lines. Grasping the role of each type is vital for maintaining an efficient, safe, and reliable plumbing system. Supply lines The integrity of plumbing supply lines is critical in delivering safe, potable water for drinking, handwashing, and patient care activities. Materials like copper, PEX, and CPVC are chosen for their durability and reliability. Flexible water supply pipes offer installation ease and adaptability, making them an excellent choice for connecting water supplies to fixtures in constrained spaces. Their construction from materials like stainless steel, PVC, or braided nylon offers durability and resistance to corrosion, ensuring reliable performance over time. Return lines Equally important are the plumbing return lines, which ensure the efficient operation and delivery of potable water systems. They contribute to patient comfort and infection control by reducing water age and stagnant conditions, preventing sediment accumulation, and ensuring temperature and disinfectant residuals. Drain and waste lines Proper sanitation in healthcare facilities hinges on effectively removing wastewater and materials through well-designed drain and waste lines. Choosing the right materials, such as PVC or cast iron, and ensuring their correct installation and maintenance are key factors in preventing backflows and the spread of pathogens. Types of plumbing material and their impact on patient safety Exploring the benefits and potential risks associated with commonly used plumbing materials—including copper, stainless steel, cast iron, galvanized steel, and various plastics such as PVC, CPVC, and PEX—helps IPs make informed decisions. PVC, CPVC, and PEX are generally not used in healthcare plumbing due to their susceptibility to biofilm formation and potential chemical leaching. These materials can create environments conducive to microbial growth, posing significant infection risks in healthcare settings. Additionally, their lower thermal tolerance and potential for chemical degradation under high-temperature water systems make them less suitable for the stringent plumbing requirements in healthcare facilities. Each material has its advantages, such as antimicrobial properties or corrosion resistance, but also considerations like the need for regular maintenance to prevent contamination. Copper Copper is favored for healthcare plumbing because of its antimicrobial qualities and durability. It lowers microbial levels in water systems and keeps water quality high with a lower risk of contamination, however over time, it can lose these properties due to scale and sediment accumulation. Used in drinkable water lines, both hot and cold, copper helps reduce infections associated with healthcare. Regular checks and maintenance are needed to avoid bacterial contamination from damaged pipes. Despite its initial cost, copper’s health advantages and long-term use can make it a cost-effective choice. Stainless steel Stainless steel is favored in healthcare for its corrosion resistance, hygiene, and durability. Its non-porous surface helps reduce bacterial growth and biofilm, promoting a cleaner water supply and helping prevent HAIs. Despite higher initial costs, its longevity and minimal replacement needs make it a cost-effective choice. Regular maintenance, including inspections and proper cleaning, is crucial for its long-term use. Stainless steel plays a vital role in maintaining patient safety in healthcare settings. Cast iron Cast iron pipes, commonly used for underground plumbing due to their durability and sound-dampening qualities, are mainly used in drainage and vent systems. Over time, these pipes may corrode, risking water contamination and health hazards. Therefore, regular checks and upkeep are crucial. Despite potential risks, when well-maintained, cast iron pipes remain a good choice for healthcare facilities, offering high crush strength and noise reduction, which is important for patient comfort. Prioritizing patient safety in healthcare plumbing material selection is key. Galvanized steel Once popular for their corrosion resistance, galvanized steel pipes can degrade over time. The zinc coating may wear off, leading to rust and bacterial growth. In healthcare settings, these pipes are unsuitable for drinking water systems due to potential water quality issues and health risks. Modern facilities prefer safer materials to reduce risks. Regular maintenance, including corrosion checks, water tests for
Plumbing 101 for Healthcare Infection Preventionists
As an infection preventionist, ensuring patient safety is a top priority. Access to clean and safe drinking water is crucial throughout patient care, making plumbing a critical component in maintaining a safe healthcare environment. In this blog, we will discuss the importance of plumbing in infection prevention, plumbing equipment associated with increased infection risk, and strategies to mitigate these risks. Common plumbing equipment in healthcare Water-bearing equipment can pose infection risks if not properly designed, maintained, and monitored. Infection preventionists should collaborate with facility staff to ensure the regular inspection and maintenance of valves and other plumbing equipment to minimize potential biofilm formation, water stagnation, and other infection risks and incorporate these activities into water management programs. Common plumbing infrastructure in healthcare facilities that can increase infection risk, include: Valves Plumbing valves such as gate valves and check valves regulate water flow and prevent backflow. They play a crucial role in controlling the direction and rate of water flow within a plumbing system. However, if not correctly sealed and maintained, valves can allow contaminants to enter the water system. They can also harbor pathogens within the biofilms that form on their inner surfaces, further increasing the risk of contaminants being introduced into the water. Valves should be regularly maintained and inspected for deficiencies to ensure proper operation. Recirculation pumps Recirculation pumps are devices used in plumbing systems to circulate hot water throughout a building. They play a key role in providing hot water quickly and efficiently to all outlets in the building. However, if not sized, installed, or maintained properly, recirculation pumps may increase the risk of infections by contributing to a favorable environment for pathogen growth. Storage tanks and water heaters Storage tanks and water heaters are crucial components of water plumbing systems, used to store and heat water for various purposes such as bathing, washing, and cooking. They are designed to maintain a steady supply of hot water at all times, ensuring convenience for the users. Tanks and heaters can harbor and contribute to pathogen growth by providing a warm water environment. This can be compounded through configurations that may lead to sediment accumulation, stagnant conditions, and temperature stratification. They pose additional risks such as leaks and corrosion if not maintained properly Water softeners Water softeners are devices designed to remove minerals such as calcium and magnesium from hard water. The purpose of using water softeners in building water plumbing systems is to prevent mineral buildup in pipes and appliances, which can reduce their efficiency and lifespan. However, water softeners may increase the risk of infections by creating an environment that promotes the growth of bacteria and other microorganisms within the water softener. If softeners are not planned or designed properly, they can also reduce disinfectant residuals, further increasing the risk of waterborne pathogens. Dead legs in pipes Dead legs in plumbing pipes are sections of pipe that do not experience sufficient flow or use. These stagnant areas of water can become breeding grounds for harmful bacteria, such as Legionella. If not effectively managed, dead legs can pose a health risk to building occupants and compromise the overall quality of the water system. Cross connection in pipes Cross connections in pipes occur when two different plumbing systems, such as a drinking water system and a non-potable water system or between the hot water system and cold water system, are connected by a common pipe. However, cross connections can pose a serious risk to building water plumbing systems by allowing water to flow between the two systems which can impact temperature delivery, disinfectant residuals, sediment levels, and even contamination of waterborne pathogens, potentially causing illness for those who consume it. Strategies for infection prevention There are various strategies to prevent infections when it comes to water-bearing equipment. All these elements above should be incorporated in the facility’s water management program, to provide a legally defensible program to mitigate the risk of waterborne pathogens. Understanding the importance of plumbing in healthcare settings is critical to preventing the spread of infections. By implementing the strategies discussed in this blog, you can help mitigate plumbing-related infection risks and foster a safe healthcare environment. Plumbing 101 group training Are you interested in a comprehensive plumbing training? LiquiTech’s group training sessions elevate your team’s knowledge, improve your water management practices, and offer the ability to earn continuing education credits, if applicable. Request the Plumbing 101 for Infection Preventionists training today.
New Study Reveals the Role of Water Systems in Mycobacteria Contamination of Medical Devices
According to a recent breakthrough study published in Nature’s Scientific Reports, researchers have successfully isolated Mycobacterium saskatchewanense from medical devices for the first time. The study identified the healthcare facility’s water system as the likely source of contamination. Mycobacterium saskatchewanense is a non-tuberculous mycobacterium (NTM) commonly found in soil and water environments. While not as well-known as Mycobacterium tuberculosis, NTMs can still pose significant health risks, especially for individuals with weakened immune systems or pre-existing health conditions. These bacteria can form biofilms and withstand chemical treatments, making them known opportunistic pathogens in healthcare facilities. The study utilized advanced identification technologies, including the GenoType Mycobacterium CM CE-IVD kit and Next Generation Sequencing (NGS). These tools allowed for precise genetic identification of the bacterium, confirming its presence on medical devices and pointing to the hospital’s water system as the likely source of contamination. The paper cited several other studies reporting elevated concentrations of mycobacteria in healthcare water systems. The plumbing systems of large structures often have areas with stagnant water, allowing biofilms to develop, which can harbor NTM. The researchers concluded that continuous and active monitoring of NTM contamination in medical devices that use water is necessary to prevent the possibility of patients becoming infected. Long-term strategies to control and prevent biofilm and Mycobacteria contamination in plumbing systems, such as through continuous disinfection of the hospital’s water system, are crucial to reducing healthcare-associated infections and ensuring patient safety. Read the full study.
Infection Prevention through Clean Water: How Healthcare Facilities Can Mitigate Healthcare-Associated Infections from Water

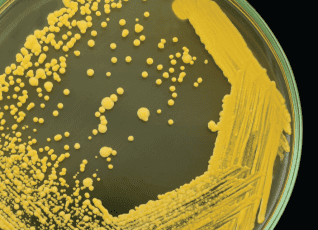
Healthcare-associated infections or HAIs are infections people get while they are receiving health care for another condition. These infections can happen in all types of healthcare settings and are a significant cause of patient illness and death. According to the Centers for Disease Control and Prevention (CDC), 1 in 31 patients experience a healthcare-associated infection on any given day, costing healthcare systems in the United States $28 billion annually. Many HAIs, including catheter-associated urinary tract infections, central line-associated bloodstream infections, surgical site infections, ventilator-associated pneumonia, and hospital-acquired pneumonia, are caused by organisms known to spread through water and biofilms. These organisms are commonly referred to as waterborne pathogens and, according to some studies, could be the cause of 20% of healthcare-associated infections. Waterborne pathogens and healthcare-associated infections Waterborne pathogens commonly linked to healthcare-associated infections include Pseudomonas, Legionella, Burkholderia, nontuberculous Mycobacteria, and Acinetobacter. Health risks associated with these pathogens can vary from mild infections to severe illnesses, and in some cases, they can even be life-threatening, particularly for high-risk individuals with compromised immune systems. Pseudomonas, Acinetobacter, Stenotrophomonas, non-tuberculous mycobacteria, and Burkholderia are bacteria frequently associated with antibiotic resistance challenges. Legionella: This bacterium thrives in water systems including cooling towers, hot tubs, and extensive plumbing systems. It is known for causing Legionnaires’ disease, a severe type of pneumonia. Pseudomonas: Found in soil, plants, and natural water sources, these bacteria can trigger serious infections in patients with compromised immune systems. Acinetobacter: These bacteria, primarily found in soil and water, have been implicated in dangerous infections in healthcare settings, particularly in patients on ventilators. Burkholderia: This group of bacteria is widely distributed in water and soil and can result in severe lung infections. Stenotrophomonas: These bacteria, found in water, soil, and plants, can lead to infections in the respiratory tract, bloodstream, and urinary system. Nontuberculous Mycobacteria: Typically present in water and soil, these bacteria can trigger lung infections in susceptible individuals, such as those with pre-existing lung conditions or suppressed immune systems. Why water quality matters in healthcare facilities Water quality plays a crucial role in healthcare facilities for many reasons, including: Approximately 20% of HAIs are caused by water. Water is everywhere in healthcare facilities. Water serves many functions in a healthcare setting and it is estimated that 65% of HAIs are associated with wet biofilm or the presence of moisture or liquid. Water is necessary to provide patient care and is used throughout the continuum of care. Hospitals treat high-risk immunocompromised patients who are at an increased risk of infection. On average, 1 in every 10 affected patients will die from their HAI. Water is not sterile. Pathogens live and grow in building water and plumbing systems, creating risk. Factors that can increase water risk Several factors can adversely impact water quality and increase the risk of healthcare-associated infections in hospitals, including water-utilizing patient equipment, water shutdowns or disruptions, and construction activities. Water-utilizing patient care equipment, such as respiratory therapy devices and wound cleaning tools, can introduce contaminants if not properly maintained and disinfected. Regular and meticulous cleaning and disinfection protocols must be in place to ensure the safety and integrity of these essential medical devices. Water shutdowns, disruptions, or events like water main breaks or flooding can compromise the water supply, leading to potential contamination and increased transmission of pathogens. It is crucial for healthcare facilities to have contingency plans and preventative water treatment systems in place, like sediment filtration, to mitigate the impact of such events on water quality. Construction and renovation activities in healthcare facilities can disturb water systems, potentially releasing harmful microorganisms and compromising the overall water quality. Adequate precautions and monitoring should be undertaken during these activities to minimize any potential risks. What organizations can do to ensure safe water quality To ensure safe water quality, healthcare organizations and healthcare professionals must prioritize clean water as part of their strategies to prevent infections. This includes implementing comprehensive control training and water management programs, conducting regular water quality testing, and maintaining water-utilizing equipment. Systemic strategies to control and prevent biofilm in plumbing systems, such as through continuous disinfection of the entire building water system, are crucial to reducing healthcare-associated infections and ensuring patient safety. References Reynolds, D., Kollef, M. The Epidemiology and Pathogenesis and Treatment of Pseudomonas aeruginosa Infections: An Update. Drugs 81, 2117–2131 (2021). https://doi.org/10.1007/s40265-021-01635-6 CDC (2021, June 21). Health Topics – Healthcare-associated Infections (HAI). https://www.cdc.gov/policy/polaris/healthtopics/hai/index.html Perkins KM, Reddy SC, Fagan R, Arduino MJ, Perz JF. Investigation of healthcare infection risks from water-related organisms: Summary of CDC consultations, 2014-2017. Infect Control Hosp Epidemiol. 2019 Jun;40(6):621-626. doi: 10.1017/ice.2019.60. Epub 2019 Apr 3. PMID: 30942147; PMCID: PMC7883772. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7883772/ World Health Organization. (2022). WHO launches first-ever global report on infection prevention and control. https://www.who.int/news/item/06-05-2022-who-launches-first-ever-global-report-on-infection-prevention-and-control Yiek, W.K., Coenen, O., Nillesen, M., & et al. (2021). Outbreaks of healthcare-associated infections linked to water-containing hospital equipment: A literature review. Antimicrobial Resistance & Infection Control, 10(77). https://doi.org/10.1186/s13756-021-00935-6
Cluster of Carbapenemase-Producing Carbapenem-Resistant Pseudomonas aeruginosa Among Patients in an Adult Intensive Care Unit
MEGAN E. CAHILL, MARTHA JAWORSKI, VICTORIA HARCY, ERIN YOUNG, D. CAL HAM, PAIGE GABLE, KRIS K. CARTERCDC, MORBIDITY AND MORTALITY WEEKLY REPORT, AUGUST 2023 IntroductionThe report discusses an examination into the infections of carbapenemase-producing carbapenem-resistant Pseudomonas aeruginosa (CP-CRPA) in an Idaho hospital (Hospital A) between September 2021 and January 2022. The infections present a significant challenge due to the high antibiotic resistance and their ability to spread from person-to-person and via environmental sources. The study focuses on two patients from the same intensive care unit room, with both isolates characterized by specific carbapenemase gene type and multilocus sequence type. ResultsThe investigative team focused on the plumbing in the ICU room because Pseudomonas aeruginosa is known to persist in biofilm, a collection of microorganisms that adhere to one another and to a surface, such as a pipe. Water samples and swabs from two sinks and one toilet were collected. CP-CRPA with the same gene type isolated in the patients was found in one of the sinks, including swab samples from the drain, p-trap (a bend in a sink drain that holds water to block sewer gases), and sink counter. Water samples from the same sink’s p-trap and a toilet also tested positive for a different strain of CP-CRPA. Due to the genetic link between the patient isolate and sink isolate, the investigative team concluded that the most likely source of the outbreak was the ICU room sink. ConclusionThe report concludes that as of December 2022, no further CP-CRPA had been reported by Hospital A, suggesting the preventative measures implemented were successful. The work highlights the importance of collaboration between healthcare facilities and public health agencies, especially in identification and response to CP-CRPA clusters in a healthcare setting. Such cooperation, alongside the implementation of robust sink hygiene interventions, is critical in controlling the spread of such resistant infections. Full report