New Study Reveals the Role of Water Systems in Mycobacteria Contamination of Medical Devices
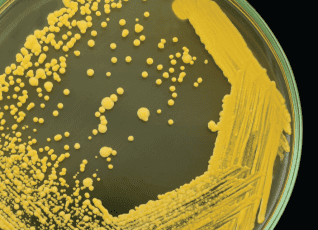
According to a recent breakthrough study published in Nature’s Scientific Reports, researchers have successfully isolated Mycobacterium saskatchewanense from medical devices for the first time. The study identified the healthcare facility’s water system as the likely source of contamination. Mycobacterium saskatchewanense is a non-tuberculous mycobacterium (NTM) commonly found in soil and water environments. While not as well-known as Mycobacterium tuberculosis, NTMs can still pose significant health risks, especially for individuals with weakened immune systems or pre-existing health conditions. These bacteria can form biofilms and withstand chemical treatments, making them known opportunistic pathogens in healthcare facilities. The study utilized advanced identification technologies, including the GenoType Mycobacterium CM CE-IVD kit and Next Generation Sequencing (NGS). These tools allowed for precise genetic identification of the bacterium, confirming its presence on medical devices and pointing to the hospital’s water system as the likely source of contamination. The paper cited several other studies reporting elevated concentrations of mycobacteria in healthcare water systems. The plumbing systems of large structures often have areas with stagnant water, allowing biofilms to develop, which can harbor NTM. The researchers concluded that continuous and active monitoring of NTM contamination in medical devices that use water is necessary to prevent the possibility of patients becoming infected. Long-term strategies to control and prevent biofilm and Mycobacteria contamination in plumbing systems, such as through continuous disinfection of the hospital’s water system, are crucial to reducing healthcare-associated infections and ensuring patient safety. Read the full study.
ASHRAE 514: A Comprehensive Guide to Safe and Efficient Building Water Systems
ASHRAE 514, released in 2023, is an ANSI Standard that establishes a comprehensive framework for ensuring the safety and management of building water systems – excluding single-family residential structures. ASHRAE 514 applies to a wide range of stakeholders, including building owners, facility managers, engineers, and water treatment professionals and requires risk management through the design, construction, commissioning, operation, repair, maintenance, replacement, and expansion of building water systems. ASHRAE Standard 514 was developed as a companion to ASHRAE 188, which provides a risk management approach to managing the risk of Legionellosis in building water systems. While the framework of ASHRAE 188 and ASHRAE 514 are similar, ASHRAE 514 expands beyond the risk of Legionella, requiring consideration of all microbial, chemical, and physical hazards associated with the building water systems. Its thorough guidelines and recommendations help in developing effective strategies for preventing and controlling waterborne diseases, safeguarding public health and improving the overall safety and well-being of building occupants. Ensuring compliance with ASHRAE 514 To maintain alignment with ASHRAE 514’s standards, it is imperative to establish a water management team and implement a comprehensive water management program to include physical, chemical, and microbial hazards. This entails performing diligent risk assessments, implementing control measures, closely monitoring the system, promptly taking corrective action when required, verifying the effectiveness of the measures, and ensuring meticulous documentation of all activities. By adhering to this comprehensive system, organizations can efficiently mitigate water-related risks, ensuring a safe and healthy environment. Tailoring water management programs To ensure effective water management, water management programs must be customized according to the specific characteristics and vulnerabilities of each building. This process considers factors such as building size, location, usage patterns, occupant risks, and specific water bearing equipment (such as water treatment). Furthermore, the water management program must undergo regular reviews and updates to identify any emerging risks or changes that may necessitate adjustments to the program. It’s advised to designate a dedicated team responsible for overseeing the program’s execution, ensuring that water systems are maintained effectively, and risks are minimized. The dedicated water management team should have a comprehensive knowledge of the building water systems as it relates to the physical, chemical, and microbial hazards of the water systems. Specific guidelines for building water systems ASHRAE 514 provides a comprehensive set of requirements for developing water management plans for building water systems. ASHRAE Standard 514 follows the same risk management approach as ASHRAE 188 and requires: Development of a program team responsible for developing and implementing the plan, A description of the building water systems and process flow diagrams that show the location of water processing steps such as heating, storing, treatment, and recirculation. Analysis of the building water systems to determine where the hazards conditions may occur and where control measures may be applied Control measures and associated control limits Monitoring procedures, frequencies, and corrective actions to take if control limit deviate from established limits. Confirmation of the plan including verification of program implementation and validation that the program is sufficiently controlling the hazard(s) Documentation and communication procedures These requirements cover identifying areas of potential risk and implementing controls to mitigate those risks effectively. There’s also the requirement for performance indicators and validation procedures to ensure the ongoing effectiveness of the water management program. Adherence to these guidelines enhances the safety and reliability of the water systems, safeguarding individuals, and communities. Design and documentation of building water systems ASHRAE 514 emphasizes the importance of integrating thorough water system management considerations from the initial design phase of a building. It stipulates that there must be detailed documentation of the water system design and installation to minimize potential risks, any changes therein, and management decisions made throughout its lifecycle. Following design and installation, ASHRAE 514 requires balancing of the building water systems to ensure proper flow and pressure, and that the startup procedures for building water system to be included, such as confirmation of operation, flushing, and disinfection of building water system. It aims to ensure the efficient and effective management of water systems in buildings, thus promoting optimal performance and risk mitigation. Additional requirements for healthcare facilities Given the heightened vulnerability of hospital occupants, ASHRAE 514 sets forth specific requirements for healthcare facilities. These requirements follow a similar water management framework but include additional considerations around patient risks and infection prevention. These provisions aim to ensure the utmost safety and well-being of patients and staff alike. Healthcare facilities must conduct comprehensive risk assessments, implement stringent control measures, and maintain robust validation and documentation procedures to track and monitor compliance. ASHRAE 514 provides a comprehensive set of standards for managing building water systems, prioritizing minimizing the risk of Legionella. Adhering to these guidelines ensures a safer and healthier environment for all building occupants.
Case Study: Copper-Silver Ionization Resolves High Bacteria Levels

In 2016 while preparing to open a new patient tower, a California hospital found bacteria levels exceeding state and federal EPA limits in the building water system. To address this issue, they deployed multiple rounds of hyperchlorination, which is the process of adding an excessive amount of chlorine to the building water system in an attempt to kill bacteria. After three unsuccessful rounds of hyperchlorination, the hospital sought the expertise of LiquiTech. LiquiTech worked with the hospital to implement a solution that included the installation of a LiquiTech™ Copper-Silver Ionization System and a LiquiTech™ Sediment Filtration System, hot water system improvements, and ongoing LiquiTech services, including proactive maintenance, monitoring, and water quality testing. After two months, the hospital’s water system test results showed bacteria levels within state and federal EPA limits, allowing the new patient tower to open. By implementing these solutions, the hospital is able to provide a safe and healthy environment for their patients, staff, and visitors. To learn more, read the full case study here.
Water Management Design Considerations for Engineers
Water management plays a pivotal role in maintaining the safety and efficiency of our buildings. As engineers and plumbing professionals, understanding the intricacies of water management best practices can guide our designs and ensure they meet industry standards. Understanding water management programs Water management programs are designed to identify and control risks in water systems that can lead to the growth of waterborne pathogens such as Legionella. High-risk conditions like water stagnation, elevated cold-water temperatures, and sediment accumulation are often the focus of these programs. Water management programs are now an industry standard for many buildings in the United States and are necessary to meet ASHRAE Standards 188 and 514, The Joint Commission, and other regulatory agencies. Developing a water management program Water management programs are site-specific and tailored to each building’s unique risks, needs, and water quality goals, and should be developed by an ASSE 12080-Certified Legionella Water Safety Specialist. The steps to developing a water management program include: Water management design considerations for engineers When designing a building water system, there are several ways that plumbing engineers and designers can incorporate water management. Here are the seven key elements of a water management program and examples of what plumbing engineers should consider for each one. Understanding and implementing these considerations in your designs ensures optimal water management and compliance with industry standards, contributing to safer buildings. Download: Water Management Guide for Plumbing Engineers Fill out the form below to download our Water Management Guide for Plumbing Engineers that includes:
Case Study: Sediment Filtration on Cold Water System Reduces Legionella Risk

After a Northeast university achieved non-detect Legionella levels in their building’s hot water system with a LiquiTech™ Copper-Silver Ionization System, they faced a new obstacle when Legionella was detected in the cold water system due to water stagnation caused by the building’s mixed-use and fluctuating occupancy. Partnering with LiquiTech, the university implemented an innovative solution to install a LiquiTech™ Sediment Filtration System on the cold water supply. By preventing sediment from entering the building, the cold water system quickly returned to non-detect Legionella levels. The combined power of copper-silver ionization for the hot water system, sediment filtration for the cold water system, and an ongoing service partnership with LiquiTech has helped the university maintain non-detect Legionella levels and provide clean, safe water to occupants. The results: With a multi-faceted approach, this university successfully controlled Legionella and proactively reduced the risk of future outbreaks. Learn more about their journey in the full case study here.
Infection Prevention through Clean Water: How Healthcare Facilities Can Mitigate Healthcare-Associated Infections from Water

Healthcare-associated infections or HAIs are infections people get while they are receiving health care for another condition. These infections can happen in all types of healthcare settings and are a significant cause of patient illness and death. According to the Centers for Disease Control and Prevention (CDC), 1 in 31 patients experience a healthcare-associated infection on any given day, costing healthcare systems in the United States $28 billion annually. Many HAIs, including catheter-associated urinary tract infections, central line-associated bloodstream infections, surgical site infections, ventilator-associated pneumonia, and hospital-acquired pneumonia, are caused by organisms known to spread through water and biofilms. These organisms are commonly referred to as waterborne pathogens and, according to some studies, could be the cause of 20% of healthcare-associated infections. Waterborne pathogens and healthcare-associated infections Waterborne pathogens commonly linked to healthcare-associated infections include Pseudomonas, Legionella, Burkholderia, nontuberculous Mycobacteria, and Acinetobacter. Health risks associated with these pathogens can vary from mild infections to severe illnesses, and in some cases, they can even be life-threatening, particularly for high-risk individuals with compromised immune systems. Pseudomonas, Acinetobacter, Stenotrophomonas, non-tuberculous mycobacteria, and Burkholderia are bacteria frequently associated with antibiotic resistance challenges. Legionella: This bacterium thrives in water systems including cooling towers, hot tubs, and extensive plumbing systems. It is known for causing Legionnaires’ disease, a severe type of pneumonia. Pseudomonas: Found in soil, plants, and natural water sources, these bacteria can trigger serious infections in patients with compromised immune systems. Acinetobacter: These bacteria, primarily found in soil and water, have been implicated in dangerous infections in healthcare settings, particularly in patients on ventilators. Burkholderia: This group of bacteria is widely distributed in water and soil and can result in severe lung infections. Stenotrophomonas: These bacteria, found in water, soil, and plants, can lead to infections in the respiratory tract, bloodstream, and urinary system. Nontuberculous Mycobacteria: Typically present in water and soil, these bacteria can trigger lung infections in susceptible individuals, such as those with pre-existing lung conditions or suppressed immune systems. Why water quality matters in healthcare facilities Water quality plays a crucial role in healthcare facilities for many reasons, including: Approximately 20% of HAIs are caused by water. Water is everywhere in healthcare facilities. Water serves many functions in a healthcare setting and it is estimated that 65% of HAIs are associated with wet biofilm or the presence of moisture or liquid. Water is necessary to provide patient care and is used throughout the continuum of care. Hospitals treat high-risk immunocompromised patients who are at an increased risk of infection. On average, 1 in every 10 affected patients will die from their HAI. Water is not sterile. Pathogens live and grow in building water and plumbing systems, creating risk. Factors that can increase water risk Several factors can adversely impact water quality and increase the risk of healthcare-associated infections in hospitals, including water-utilizing patient equipment, water shutdowns or disruptions, and construction activities. Water-utilizing patient care equipment, such as respiratory therapy devices and wound cleaning tools, can introduce contaminants if not properly maintained and disinfected. Regular and meticulous cleaning and disinfection protocols must be in place to ensure the safety and integrity of these essential medical devices. Water shutdowns, disruptions, or events like water main breaks or flooding can compromise the water supply, leading to potential contamination and increased transmission of pathogens. It is crucial for healthcare facilities to have contingency plans and preventative water treatment systems in place, like sediment filtration, to mitigate the impact of such events on water quality. Construction and renovation activities in healthcare facilities can disturb water systems, potentially releasing harmful microorganisms and compromising the overall water quality. Adequate precautions and monitoring should be undertaken during these activities to minimize any potential risks. What organizations can do to ensure safe water quality To ensure safe water quality, healthcare organizations and healthcare professionals must prioritize clean water as part of their strategies to prevent infections. This includes implementing comprehensive control training and water management programs, conducting regular water quality testing, and maintaining water-utilizing equipment. Systemic strategies to control and prevent biofilm in plumbing systems, such as through continuous disinfection of the entire building water system, are crucial to reducing healthcare-associated infections and ensuring patient safety. References Reynolds, D., Kollef, M. The Epidemiology and Pathogenesis and Treatment of Pseudomonas aeruginosa Infections: An Update. Drugs 81, 2117–2131 (2021). https://doi.org/10.1007/s40265-021-01635-6 CDC (2021, June 21). Health Topics – Healthcare-associated Infections (HAI). https://www.cdc.gov/policy/polaris/healthtopics/hai/index.html Perkins KM, Reddy SC, Fagan R, Arduino MJ, Perz JF. Investigation of healthcare infection risks from water-related organisms: Summary of CDC consultations, 2014-2017. Infect Control Hosp Epidemiol. 2019 Jun;40(6):621-626. doi: 10.1017/ice.2019.60. Epub 2019 Apr 3. PMID: 30942147; PMCID: PMC7883772. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7883772/ World Health Organization. (2022). WHO launches first-ever global report on infection prevention and control. https://www.who.int/news/item/06-05-2022-who-launches-first-ever-global-report-on-infection-prevention-and-control Yiek, W.K., Coenen, O., Nillesen, M., & et al. (2021). Outbreaks of healthcare-associated infections linked to water-containing hospital equipment: A literature review. Antimicrobial Resistance & Infection Control, 10(77). https://doi.org/10.1186/s13756-021-00935-6
Legionella Risk Assessment: Essential Information for Building Owners and Managers

Legionella is a type of bacteria that can cause Legionnaires’ disease, a severe form of pneumonia. Unfortunately, Legionella can be found in any building, including hospitals, skilled nursing facilities, hotels, and office buildings. The good news is that there are steps you can take to identify and manage the risks associated with Legionella. What is a Legionella risk assessment? A Legionella risk assessment is a process that identifies the potential for Legionella bacteria to grow and spread through water systems within a building. This assessment should be conducted by an ASSE 12080 Certified Legionella Water Safety and Management Specialist and include: Fill out the form at the bottom of this page to download our Legionella Risk Assessment template for a detailed list of what an assessment should include. Who needs a Legionella risk assessment? Since Legionella can colonize any type of building, all buildings with potable water systems and aerosol-generating systems (such as cooling towers) should conduct a Legionella risk assessment to determine potential risks to building occupants and potential sources of Legionella transmission. This is especially true for hospitals, skilled nursing facilities, office buildings, hotels, and any building with a water system at risk of Legionella contamination. Landlords, building owners, and employers are responsible for protecting their occupants from Legionella exposure. How often do you need to conduct a Legionella risk assessment? Legionella risk assessments should be conducted annually or even more frequently if recommended by a water safety specialist. Additionally, any changes to the building’s water system should trigger a reassessment to address Legionella risks proactively. What are the benefits of conducting a Legionella risk assessment? Regular Legionella risk assessments provide numerous benefits: To ensure the health and well-being of occupants and minimize risk, buildings with water systems must undergo regular Legionella risk assessments. Don’t wait for a Legionella outbreak to occur – contact our ASSE 12080 Certified Legionella Water Safety and Management Specialists to schedule your Legionella risk assessment today. Download: Legionella Risk Assessment Template Fill out the form to download our Legionella Risk Assessment template for a detailed list of what an assessment should include.
Controlling Legionella Case Study: Chlorine Dioxide vs. Copper-Silver Ionization

In 2009, an outbreak of Legionnaire’s Disease hit a large Georgia hospital, affecting six wards, and resulting in the closure of 10% of their patient beds. After trying several solutions, including installation of continuous chlorine dioxide systems and plumbing infrastructure upgrades, the hospital still tested positive for Legionella. In 2023, the hospital partnered with LiquiTech to install a LiquiTech™ Copper-Silver Ionization System to control the Legionella contamination and reduce the risk of future disease outbreaks. Within just two months of installing copper-silver ionization, the Legionella positivity rate dropped from 100% to 11%, with the next round of testing showing 0% positivity. Through its ongoing service partnership with LiquiTech, the hospital has successfully maintained control of the Legionella contamination. By choosing the right technology and ensuring ongoing maintenance, the hospital’s priorities of protecting their staff and patients and controlling waterborne pathogens were achieved. To learn more, read the full case study here.
Sediment in Building Water Systems: How It Impacts Plumbing and Budget

Sediment in your building’s water system can cause damage to plumbing, increase maintenance costs, and promote bacterial growth. To ensure your building water system runs smoothly and efficiently, it’s crucial to understand what sediment is, how it enters your water system, and strategies to control it. Sediment in building water systems Sediment is a naturally occurring material that gets into source water from soil runoff or the breakdown of organic materials. It can get into a building’s water system from: Sediment’s impact on plumbing Too much sediment in a building’s water system can damage plumbing, increase operational costs, and reduce the life expectancy of equipment, including: Sediment’s impact on bacterial growth High sediment loads can encourage bacterial growth, increasing a facility’s risk of disease outbreak, like Legionnaire’s Disease. Three key ways sediment increases bacterial growth include: Benefits of controlling sediment in building water systems The benefits of controlling sediment in your building water system include: How to control sediment in building water systems There are several ways facilities can control sediment in their building water system, including: Sediment filtration case study A newly built facility in Colorado began experiencing issues with its plumbing infrastructure soon after opening its doors to patients in 2016, including: A sediment test by LiquiTech uncovered 26 times the World Health Organization-recommended sediment levels entering the building from the incoming water supply. Installing a new LiquiTech Sediment Filtration System removed 96.7% of incoming sediment, helping the facility: Installing a sediment filtration system is an effective way to control sediment, improve water quality, and extend the life of plumbing equipment. It can also result in cost savings for facilities by reducing maintenance and equipment replacement costs. For more insights on controlling sediment in your building water system, contact us today. Our team of ASSE 12080 Certified Legionella Water Safety and Management Specialists can work with you to develop a solution that’s tailored to your specific needs.
CDC Report Links Cluster of Healthcare-Associated Infections to Water System
A report published in CDC’s Morbidity and Mortality Weekly Report on August 4, 2023 linked a cluster of healthcare-associated infections to an Idaho hospital’s potable water system. According to the report, two patients who stayed in the same ICU room four months apart were found to be infected with carbapenemase-producing carbapenem-resistant Pseudomonas aeruginosa (CP-CRPA). Carbapenem-resistant organisms, such as CRPA, are gram-negative bacteria resistant to the carbapenem class of antibiotics, a broad-spectrum antibiotic considered a “last resort.” Certain carbapenem-resistant organisms are resistant because they produce carbapenemase enzymes that make carbapenems ineffective. Infections from carbapenemase-producing organisms are difficult to treat and associated with high mortality. Pseudomonas aeruginosa can carry genes encoded with carbapenemases that can be transferred between strains and across bacterial species, leading to the spread of antibiotic resistance. CP-CRPA infections are typically transmitted from person-to-person or acquired from environmental sources, like water, sink drains, and toilets. Investigation and resultsA collaborative investigation involving the Idaho Division of Public Health, the Idaho Bureau of Laboratories, the Utah Public Health Laboratory, and the CDC was undertaken to identify the cause of the infection. The investigative team focused on the plumbing in the ICU room because Pseudomonas aeruginosa is known to persist in biofilm, a collection of microorganisms that adhere to one another and to a surface, such as a pipe. Water samples and swabs from two sinks and one toilet were collected. CP-CRPA with the same gene type isolated in the patients was found in one of the sinks, including swab samples from the drain, p-trap (a bend in a sink drain that holds water to block sewer gases), and sink counter. Water samples from the same sink’s p-trap and a toilet also tested positive for a different strain of CP-CRPA. Due to the genetic link between the patient isolate and sink isolate, the investigative team concluded that the most likely source of the outbreak was the ICU room sink. Prevention and control measuresUpon identifying the sink as the likely infection source, suggested measures for prevention and control were immediately instituted. These included the application of biofilm disinfectants, a screening regimen for future patients occupying the room, and a commitment towards forwarding any CP-CRPA isolates to public health laboratories for detailed molecular profiling, prevention, and control. On conducting a retest, no further CP-CRPA strains were detected in the environmental samples. As of December 2022, no additional CP-CRPA isolates have been reported by the hospital. These findings underpin the important relationship between biofilm, building water systems, and healthcare-associated infections. Long-term strategies to control and prevent biofilm in plumbing systems, such as through continuous disinfection of the entire building water system, are crucial to reducing healthcare-associated infections and ensuring patient safety. Read the full report. ReferencesCenters for Disease Control and Prevention. (2023). Carbapenemase-Producing Organisms (CPO). Carbapenemase-Producing Organisms (CPO) 2023 Case Definition | CDC Minnesota Department of Health. (2023). Carbapenem Resistant Pseudomonas aeruginosa (CRPA). Carbapenem Resistant Pseudomonas aeruginosa (CRPA) – MN Dept. of Health (state.mn.us) Centers for Disease Control and Prevention. (2023). Cluster of Carbapenemase-Producing Carbapenem-Resistant Pseudomonas aeruginosa Among Patients in an Adult Intensive Care Unit. Morbidity and Mortality Weekly Report | CDC